- WHAT EVERY MAN SHOULD KNOW
- CAUSES OF INFERTILITY
- UNDERSTANDING
HUMAN REPRODUCTION
- HOW DO SPERM MATURE
- EGG AND SPERM
- FACTORS DETERMINING FERTILITY
- THINGS AFFECTING ABILITY TO CONCEIVE
- NOTE OF CAUTION
- GETTING HELP
FOR INFERTILITY
- SEMEN ANALYSIS
- LABORATORY TESTING
- SURGICAL THERAPY
- MEDICAL THERAPY
- TREATING
- ASSITED REPRODUCTIVE TECHNOLOGIES
- CONCLUSION
 |
What every man should know |
 |
The inability to concieve comes as a surprise to most men and women, many of whom have no medical history to suggest a fertility problem. Most couples approach childbearing with the thought that once the use of birth control is stopped, pregnancy will immediately follow. Although, this happens for many couples without too much difficulty, others soon discover that having a baby is not so simple after all.
Difficulty in conceiving is surprisingly common, affecting about 1 couple in 12, or about 8% of the population. Infertility is defined as the inability of a couple to achieve conception after a year of unprotected intercourse ( or 6 months if the woman is over age 35 ) or the inability to carry a pregnancy to alive birth.
|
There are two general types of infertility. Difficulty in conceiving for a couple who has never had a baby before is defined as primary infertility. Secondary infertility is defined as the inability to become pregnant again when the same partner has already had a baby. |
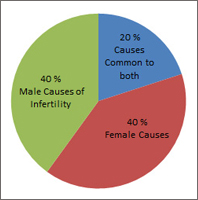
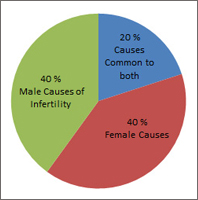
Historically, infertility has largely been attributed to the female. However, in reality, it affects men and women almost equally. Female related factors account for 40% of infertility, with male related factors accounting for another 40%. A combination of male and female related factors account for about 10% of infertility, while the remaining 10% of infertility is due to unexplained causes. Thus, the male may contribute to infertility in about 50% of couples. Therefore, it is important for both parents to understand the problems and discuss treatments with their doctors as a couple.
Male infertility may be caused by a number of factors, including problems with sperm production, blockage of the sperm delivery systems, antibodies against sperm, injury to the testicle, problems relating to hormone production, anatomical problems or the presence of a varicose vein around the testicle ( varicocele ) - all of which may affect sperm quality and quantity. Past illnesses, infections, various diseases and medications can also cause infertility.
Whatever the cause, coping with infertility is never easy. Many men believe that society views infertility as a sign of inadequacy and thus, may suffer from feelings of poor self - esteem. Some men feel robbed of their masculinity and virility as well. These feelings are normal. The key to resolving these issues is communication. Whether the difficulty in conceiving is related to the male or female, infertility should be approached as a couple's shared challenge. Supporting each other and working together can strengthen the relationship while overcoming the challenge of infertility.
It is important to note that about 70 - 80 % of all infertility can be traced to specific causes that can be treated. Many treatment options are available to treat male infertility. These options range from medical therapy to surgical procedures, and success rates are steadily improving.
 |
Causes of Infertility |
|
| |
|
 |
|
| |
| |
 |
Varicocele |
 |
Endocrinologic |
 |
Idiopathic |
 |
Infection |
 |
Obstruction |
 |
Sexual Dysfunction |
 |
Normal / Female Factor |
 |
Systematic Disease |
 |
Cryptorchidism |
 |
Sertoli Only |
 |
Immunologic |
 |
Ultrastructural Defect |
 |
Ejaculatory Dysfunction |
 |
Genetic |
 |
Drug / Radiation |
 |
Testis Cancer |
|
 |
Understanding Human Reproduction |
|
| |
Human reproduction is surprisingly inefficient. The likelihood of pregnancy within any given month is believed to be about 25%. For this reason, it is important to realize that having a baby is quite complex and involves the fertility of both partners. This is why it is important to understand the normal reproductive functions in both men and women. |
| |
 |
Hormonal Functions |
|
| |
In the male, the production of reproductive hormones is central to fertility, and pituitary hormones initiate the sperm production process. The pituitary gland secretes follicle stimulating hormone (FSH) and luteinizing hormone (LH). These are the same hormones necessary for regulating the female's reproductive functions too. In men, FSH stimulates the production of testosterone, the male hormone that helps maintain spermatogenesis, as well as the male's sexual characteristics. |
 |
How do sperm mature |
|
| |
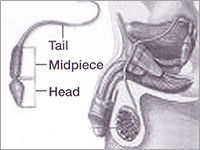
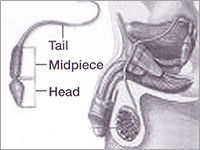
Sperm develop in specialized cells called sertoli cells, which are found within the seminiferous tubules within the testes. The developmental process of the sperm begins with the division of very immature cells (spermatogonia) and proceeds through several stages to maturity. Mature sperm are tadpole - shaped and referred to as spermatozoa. Spermatozoa leave the seminiferous tubules to pass into the epididymis where they acquire the ability to move. Eventually the long whip like tails help propel sperm through the female reproductive tract. |
| |
 |
What happens next |
|
| |
Mature sperm remain in the vas deferens (in the widened upper end called the ampulla) until the man ejaculates or expels fluid from his penis during intercourse. As the man ejaculates, sperm combines with fluid from the seminal vesicle and with a thick secretion from the prostat gland thus creating semen. This fluid (or ejaculate) is discharged through the erect penis and deposited into the woman's vagina. At the time of ejaculation, semen is gel - like and liquified within 5 to 30 minutes. The liquefaction enables the sperm to more effectively swim through the female reproductive tract and reach the ovem (egg). |
 |
The Egg and the Sperm |
|
| |
|
 |
Each month, a single egg matures inside a follicle (cyst like structure) within an ovary. Ad midcycle, the egg is released from the follicle (ovulation). The egg then travels down one of the fallopian tubes towards the uterus. It is at the end of the fallopian tube, near the uterus, that the fertilization of the egg usually occurs.
It is important to understand that contact of egg and sperm is a highly random event. As mentioned previously, the chance of conception is at best only about 25% in any given month, even under the best conditions.
|
| If fertilization does not occur, the uterus will shed its lining, thus beginning the woman's period and starting the next menstrual cycle. The egg simply passes through the uterus and is flushed from the woman's body.
Normally, millions of sperms are deposited into the vagina. However, as they swim through the cervix and uterus, up to the fallopian tube, their numbers decline. Only a few hundred sperms will get close to the egg. Sperms must then be able to penetrate and fertilize the egg. Although, several sperms will try, only one will be successful. Sperms are able to survive for 2 to 3 days within the female's reproductive tract.
The length of time that a woman's egg can be fertilized by a man's sperm ranges from 12 to 24 house. |
|
 |
Factors that determine the ability of sperm to fertilize an egg |
|
| |
 |
Volume of semen (the total amount of ejaculate) |
| |
|
 |
Sperm count or density (the number) |
| |
|
 |
Sperm motility (the ability to move) |
| |
|
 |
Forward progression (the quality of movement) |
| |
|
 |
Sperm forms (the size and shape) |
| |
|
| Although sperm count is critical, sperm motility and forward progression appear to be more important factors in determining the fertilizing capacity of sperm. Despite a low sperm count, many men with high quality (viable and highly motile) sperm may still be fertile. |
| |
|
 |
Factors that influence Fertility |
|
| |
|
| A man's overall health can have a significant impact on his fertility. This is why it is important for a couple to take good care of themselves when they are trying to conceive. |
|
 |
Several things can effect the ability to conceive |
|
| |
|
 |
Note of Caution |
|
| |
Any or all of the following conditions warrant seeing a doctor without delay if a man has been unsuccessful achieving pregnancy with his partner.
 |
A history of sexually transmitted diseases |
| |
|
 |
A history of drug, alcohol or cigarette abuse |
| |
|
 |
Previous urologic surgery |
| |
|
 |
Any sexual difficulties |
| |
|
 |
Mumps (after puberty) |
| |
|
 |
Vasectomy reversal |
| |
|
 |
Prostate infections |
|
 |
Getting Help for Infertility |
|
| |
When a couple has been having unprotected intercourse for a year or more without achieving pregnancy (or 6 months if the female partner is over the age of 35), one or both of the partners may be infertile. If a couple meets the definition of infertility, it is important to seek medical attention as soon as possible. The earlier the problem is detected, the better the chances for successful treatment. There is user friendly Andrology OPD at IVF Pune, Deenanath Mangeshkar Hospital. Please use the facility. |
| |
 |
The Infertility Evaluation |
|
| |
| The process used to identify fertility problems is referred to as the infertility work up. The basic work up for men is composed of three elements and is generally performed simultaneously in both partners. |
| |
 Medical History Medical History |
The doctor will want to know as much about the man's medical history as possible. Special attention is paid to specific areas that may affect fertility but might escape notice in a routine medical interview. These areas include : sexual practices (secual interest / desire), use of lubricants and the timing and frequency of intercourse), prior pregnancies (with past or present partner) and previous infertility work-ups and treatments. A history of disease or illnesses (such as viral infections, fevers or diabetes mellitus) will be reviewed. The medical history will also cover childhood and developmental history, including questions about any testicular abnormalities or groin injury after the onset of puberty. Other factors that may be important include a history of exposure to chemicals or radiation while on the job or elsewhere, exposure to heat (such as the regular use of hot tubs or saunas), any recent illness accompanied by a high fever or the use of medications or recreational drugs. |
| |
 Physical Examination Physical Examination |
The male infertility evaluation also includes a thorough physical examination with emphasis on the external reproductive organs and secondary sex characteristics. Size and firmness of the testes are evaluated, as well as possible obstruction of epididymis. The scrotum is evaluated for varicoceles, which doctors can feel during the examination. Approximately 25% to 30% of infertile men have a varicocele, usually on the left side. Ultrasound and x-rays are sometimes used to identify smaller varicoceles, but a careful physical examination is the most common method of detection. An additional part of the examination may involve an examination of the prostate gland and seminal vesicles. |
 |
Semen Analysis |
|
| |
A semen analysis is the study of a freshly ejaculated semen sample. This analysis measures the number of sperms present in the ejaculate (sperm counts) and checks the shape and size (morphology) of sperm and their motility.
Semen testing is performed using a fresh semen specimen within 2 hours of collection. This test is done by a certified laboratory. The specimen is obtained through masturbation and is collected in a sterile container. Semen for this analysis should not be obtained by interrupted intercourse or by use of an ordinary condom. Ordinary condoms contain substances that are toxic to sperm. If the religious or personal practices prohibit masturbation or if the patient feels uncomfortable, the doctor may suggest using a special condom designed for specimen collection that does not damage sperm. Feeling anxious about producing a specimen is common. Any questions or concerns should be discussed with a doctor.
The information gathered during the semen analysis depends on proper collection of the specimen, as well as the skill of the technician performing the test. Before testing, a standard period of secual abstinence is recommended of 2 to 5 days. Because sperm counts and quality can vary, at least two samples will usually be obtained to establish a baseline.
Evaluation of semen is b ased on standards established for fertile males (refer below). When a patient has values below these limits, a male factor does not necessarily exist, but the probability is significantly increased. It is important to remember that, despite an overall low sperm count, men with high quality sperms may still be fertile. High quality sperm is defined as having a high percentage of motile sperms with good forward movement. Sperm motility appears to be one of the most important factors in determining the fertilizing capability of sperm. |
| |
 Standard Parameters Commonly Used to define normal Semen Analysis on atleast two occasions Standard Parameters Commonly Used to define normal Semen Analysis on atleast two occasions |
| |
|
|
| - |
Volume |
2.0 mL to 5.0 mL or more |
| |
|
|
| - |
Sperm number |
20 million / mL or more |
| |
|
|
| - |
Motility |
50% or more with good forward progression |
| |
|
|
| - |
Morphology |
30% or more normal forms |
| |
|
|
| |
And :
- No significant sperm clumping.
- No significant white blood cells or red blood cells.
- No hyper viscosity (increased thickening of the seminal fluid)
In the event of the sperm count being normal no further tests are required to analyse the fertility of the male. However if an abnormality is found in the semen sample in terms of low counts or decreased motility or the presence of abnormal looking sperms then further tests are warranted. |
|
 |
Laboratory Testing |
|
| |
 Endocrine Tests Endocrine Tests |
Blood tests to measure circulating hormones can reveal valuable information about testicular function and causes of infertility. FSH and LH are both involved in the maintenance of sperm development and testosterone levels. LH stimulates the production of testosterone, whereas FSH is a sensitive indicator of normal sperm production. |
| |
 Ultrasound examination of the testes Ultrasound examination of the testes |
Sometimes ultrasound examination of the testes and the epididymis as well as the other male reproductive organs is carried out. This is useful to determine the size of the testes and to give an idea about any block in the male reproductive tract. Ultrasound examination is also useful to rule out a varicocele. |
| |
 Testicular Biopsy Testicular Biopsy |
A testicular biopsy is used to determine the ability of the sperm producing cell to produce normal sperms. It allows a direct inspection of the testicular tissue. This is then examined under a microscope for signs and patterns that suggest why sperm counts are abnormal. On performing a testicular biopsy a clear idea is obtained regarding the pathology within the testis and the chance of finding viable sperms for use in Assisted Reproduction (ICSI) can also be determined. If sperms are found these can then be used for fertilizing the wife's oocytes by a method called ICSI. Thus testicular biopsy helps not only in diagnosis but also as a therapeutic option in Assited Reproduction. |
| |
 |
Surgical Therapy |
|
| |
Treatment of male infertility may require surgery or medication or may involve in vitro techniques for improving the quality of sperm. Several methods of treatment are available.
Surgical therapy in the treatment of male infertility is aimed at improving the production of sperm or improving its delivery from the testes and epididymis to the egg. When a blockage is identified, several procedures may be performed to correct the obstruction and enable normal sperm delivery. Some surgical procedures, like varicocele repair, do not directly improve sperm transport pathways, rather these operations help to improve the sperm production process. There are several surgical procedures that the doctor may suggest, depending on the patient's specific situation. Some procedures are performed to both diagnose and treat a problem, if found. However there are times when surgical repair is not possible and even when the repair is possible the probability of achieving a cure and then a pregnancy is around 40% over the next year or two. Hence in cases where the woman's age is already advanced, Assisted Reproductive techniques like IVF and ICSI are still preferred over surgical treatment. |
| |
| Therapeutic surgical procedures which are done are as follows : |
| |
 Varicocele Repair Varicocele Repair |
The role of varicoceles in male infertility is controversial. However when varicoceles are associated with decreased sperm motility especially in cases of secondary infertility, and when abnormalities in semen quality cannot be explained by other causes, then surgical correction of varicocele may help and is carried out. In addition the presence of testicular pain or loss of testicular size (atrophy) in the presence of varicocele are also compelling reasons to recommend correction. |
| |
 Vasovasostomy Vasovasostomy |
This procedure surgically repairs the vas deferns, and is generally used to reverse the vasectomy (male sterilization procedure) that the man may have undergone. Surgical correction for other vasal blockages such as those caused by infection can also be done after a proper evaluation. |
| |
 Epididymovasostomy Epididymovasostomy |
This means creation of a new connection between the vas deferens and the epididymis. This is a microsurgical procedure and is done after confirming the site of obstruction. However surgical correction of an obstruction in such cases is not always possible and even in cases where it is done the success rates vary between 30 - 50%. |
 |
Medical Therapy |
|
| |
Men seen for evaluation of infertility may have a hormonal disorder that can be treated with medical therapy. These disorders include hypogonadotrophic hypogonadism (lack of hormone production, which results in an inability to produce sperm) and hyperprolactinemia (an increased presence of prolactin in the body).
Most conditions of diagnosed hyperprolactinemia are unexplained, with the cause unknown. Highly specific therapy (bromocriptine, cabergolin) is availabe as a treatment measure. However, pituitary tumors can also cause elevated prolactin. Medical treatment should not be started without an MRI or CT scan of the pituitary gland. |
 |
Treating Antisperm Antibodies, Infections and Unexplained Oligospermia |
|
| |
 Treating Antisperm Antibodies Treating Antisperm Antibodies |
Antisperm antibodies may be the reason for sperms of adequate density but with impaired motility. Antisperm antibodies interfere with sperm function, causing sperms to clump togethre, lose motility or lose the ability to fertilize an egg. Suppression of these antibodies with medical treatment has been reported to improve semen quality with variable success. Treatment may include certain types of steriods (eg prednisone), sperm washing and intrauterine insemination, or in vitro fertilization, especially if combined with intracytoplasmic sperm injection (ICSI), the injection of sperm into the egg. |
| |
 Treating Infections Treating Infections |
Male infertility may also be caused by infection of th sex accessory glands (prostate, seminal vesicles, etc). Some bacteria may cause obstructive azoospermia because they attack the testes or epididymis, and may cause permanent sterility due to scarring. In some cases, infections that reside primarily in the prostate or seminal vesicles may cause little or no symptoms and have questionable impact on a man's fertility potential. Still other infection, particularly those involving the prostate, may have no symptoms but will reduce sperm motility. Antibiotics are best used only when a specific infectious agent can be identified. |
| |
 Treating Unexplained Oligospermia Treating Unexplained Oligospermia |
Some men who present with infertility have normal male anatomy, a normal hormone profile and no apparent reason for their poor semen analyses. These patients, who are classified as having idiopathic (unexplained) oligospermia, may be treated with medical regimens. Additional candidates for medical therapy include those noted to have idiopathic asthenospermia (a decrease in sperm movement with no known reason), those who fail to improve after varicocele repair and those who fail to achieve adequate semen quality after vasectomy reveral despite the presence of sperm in the ejaculate. Men with unexplained infertility should discuss the available treatment options with their doctor. |
 |
Assited Reproductive Technologies |
|
| |
| Assisted Reproductive Technologies (ART) offers an alternative for those who have been unsuccessful in previous attempts to have a baby and is used for men who have failed to respond to surgical and medical treatment for known treatable causes of impaired sperm quality and quantity. |
| |
| ART includes procedures such as : |
 |
Intrauterine Insemination (IUI) |
 |
Donor Insemination (DI) |
 |
In Vitro fertilization (IVF) |
 |
Micromanipulation |
 |
Intracytoplasmic sperm injection (ICSI) |
|
| |
 Intrauterine Insemination (IUI) Intrauterine Insemination (IUI) |
| |
|
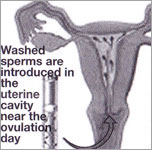 |
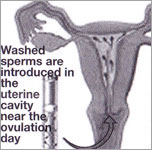
Intrauterine insemination (IUI), a type of artificial insemination with the male partner's sperm, involves the placement of large numbers of processed (washed and concentrated), motile sperms high inside the uterus during the most fertile time of the female's menstrual cycle (midcycle). This procedure bypasses certain natural barriers within the female reproductive tract, most notably the cervix, and is used in couples with a cervical factor (cervicitis, cervical stenosis, inadequate mucus or hostile mucus), unexplained infertility, male factor infertility or immunologic infertility. Pregnancy rates vary, and the outcome is highly dependant on the initial reason for treatment. Generally when IUI is carried out along with some form of ovarian stimulation using drugs like clomiphene and gonadotropins the success rates are better.
|
IUI is performed in the clinic without anaesthesia. The doctor or nurse inserts sperm directly into the female reproductive tract, near the time of ovulation, so that the sperm will reach the egg and fertilize it. Sometimes, more than one insemination per cycle is performed to ensure that insemination coincides with ovulation. |
|
| |
 Donor insemination (DI) Donor insemination (DI) |
If the male partner suffers from severe problems or does not have any sperm, the doctor may suggest therapeutic insemination by a donor. A donor may also be suggested if the male partner carries a genetic disorder. Fresh samples are no longer used in donor insemination. Before insemination, donor sperm are first frozen at least 6 months and stored. This enables adequate screening and helps to prevent the spread of communicable diseases. If donor insemination is suggested, you need not make a decision right away. Using donor sperm requires a period of adjustment for both partner. |
| |
 Additional reasons to use DI Additional reasons to use DI |
| - |
Infertility |
| - |
No sperm count |
| - |
Ejaculation problems |
| - |
Defects in sperm function |
| - |
Genetic incompatibility |
|
| |
 In Vitro Fertilization (IVF) In Vitro Fertilization (IVF) |
In Vitro Fertilization (IVF) was originally developed as an alternative means of fertilizing an egg when it was not possible for the sperm to reach the egg in the normal way (through the female's fallopian tubes) due to irreversible tubal damange.
IVF involves placing the couple's sperm and egg together in a laboratory dish to fertilize in vitro (outside the woman's body), and then placing the fertilized eggs into the uterus. IVF is also being used as a treatment option for selected males. Embryos fertilized with sperms from males with semen of reduced quality seem to have a chance of implanting that is as good as if not better than that of embryos fertilized with sperm from men with normal semen. |
| |
 Micromanipulation Micromanipulation |
This procedure involves standard IVF combined with procedures directed at increasing the change of fertilization, especially for men with very low sperm counts or for couples who have not been successful with routine IVF. |
| |
 Intracytoplasmic Sperm Injection (ICSI) Intracytoplasmic Sperm Injection (ICSI) |
Pioneered in Belgium, ICSI is the newest micromanipulation procedure and is a promising new treatment for male infertility. This laboratory technique involves the injection of a single sperm into the very substance of the egg, bypassing both the need to have the sperm swim through the reproductive tract to reach the egg and the need to have the sperm penetrate the egg. The female partner will undergo ovarian stimulation and egg recovery in preparation for micromanipulation and embryo transfer.
ICSI may provide men who produce very low amounts of weak sperm a chance to establish a pregnancy. ICSI is also routinely used in cases of azoospermia where sperm can be available in the testes. Thus the sperm used for ICSI can be obtained, (regardless of how it is obtained) it is injected directly into the egg. Eggs that fertilize are then transferred to the female partner's uterus, just as in an IVF cycle. The success rate can be as high as 35%. |
 |
Conclusion |
|
| |
Despite the significant advances in treatment, infertility can have a great emotional impact and can test even the strongest relationships. Infertility leaves many men feeling a loss of control over their self image, secual and emotinal well being and ability to handle a crises. Partner may cope in different ways and at different times as they each struggle with infertility. As a result, the sexual relationship may be affected. |
| |
|
 |
Dealing with infertility can be emotionally demanding. Health professionals have found that communicating one's own feelings and understanding those of one's partner can help relieve some of the stress and frustration. Couples should try to support each other and should not hesitate to seek outside help. A qualified counselor is also available at our clinic to help you through this trying time. In fact 65% of infertile couples who seek medical help eventually succeed in having children through a variety of medical procedures and treatment available today.
|
Although treatment of infertility can be a stressful process, it is important to remember that no one is to blame for any failure to respond to therapy. There is hope. |
|
| |
At some point, couples will need to put closure on infertility. If infertility therapy has not been successful, some couples choose to fulfill their family building goals through adoption. Others may choose not to have children and pursue other outlets for their emotional and nurturing energies. What seems most helpful is successfully working through the difficult and consuming feeling of the infertility experience, a couple can face the challange of infertility successfully, only by approaching the situation together. Their survival of the emotional, mental and physical stress of infertility can result in a strengthened relationship.
Many couples find that as result of working together to overcome infertility they are closer to their partners than ever before. Working together can be an emotionally rewarding journey for the couple and it couldmean starting to live life all over again. |
|
 MALE INFERTILITY
MALE INFERTILITY